Integrating the Healthcare Enterprise
IHE IT Infrastructure White Paper
mCSD White Paper
Revision 1.1 - Published
Date: November 8, 2021
Author: ITI Technical Committee
Email: iti@ihe.net
Foreword
This is a white paper of the IHE IT Infrastructure (ITI) domain.
This white paper is published on November 8, 2021. Comments can be submitted via traditional methods at ITI Public Comments or by creating a GitHub Issue. Please reference the section that your comment applies to.
General information about IHE can be found at https://www.ihe.net.
Information about the IHE IT Infrastructure domain can be found at https://www.ihe.net/IHE_Domains.
Information about the organization of IHE Technical Frameworks and Supplements and the process used to create them can be found at https://www.ihe.net/about_ihe/ihe_process and https://www.ihe.net/resources/profiles.
The current version of the IHE IT Infrastructure Technical Framework can be found at https://profiles.ihe.net/ITI/TF/index.html.
CONTENTS
- 1 Introduction
- 2 Key Use Cases
- 3 Facility Registry
- 4 Health Worker Registry
- 5 Care Services Registry
1 Introduction
This white paper describes some common uses where the Mobile Care Services Discovery (mCSD) Profile can be used to help implementation of services discovery using registries or directories. In general, registry services are designed to uniquely identify and track unique patients, facilities, healthcare products and terminology that are used throughout the health information exchange.
A core need in health information exchange is to have common, authoritative registries of locations, organizations, jurisdictions, practitioners, and the roles and services they offer. These services can be discoverable using mCSD. mCSD provides extensions of the core FHIR® resources to support health information exchange across the enterprise, including the queries and updates that legacy systems must support to access authoritative registries. For example, an electronic medical records (EMR) system with the ability to perform care services discovery can help patients get the care they need, from a licensed practitioner, in a location where it is provided.
mCSD also provides extensions that support diverse funding mechanisms and attribution for reporting. mCSD supports complex organizational hierarchies. For example, the mCSD extension for the Organization resource allows for more than one parent Organization resource. This is powerful in that is supports a health facility to be in the hierarchy of several organizations, for example different departments in the same Ministry of Health.
The mCSD implementation guide can be used in various configurations, each suited for a different use case. The variations will be discussed in the context of these common use cases. This white paper further outlines several use cases that can be adapted to many contexts, including creating facilities and health worker registries.
1.1 Scope
Effective health information exchange involves a diverse set of activities and a broad set of challenges, whether that exchange takes place among affiliated or unaffiliated care providers. The IT Infrastructure (ITI) domain of IHE has addressed many of these challenges by defining a series of integration profiles to address specific aspects of exchanging healthcare information. Each integration profile addresses part of the broad set of challenges involved in health information exchange. The profiles; however, do not attempt to address governance and policy choices that significantly affect how the profile is adapted in any particular community. This white paper cannot address all such governance and policy issues but will provide some guidance on where governance and policy issues are applicable and offer some common approaches.
It is very important to note that IHE focuses only on interoperability and does not attempt to solve every issue involved in exchanging health information. These solutions are meant to be plugged into an architecture that is designed and executed by the exchange communities themselves. Thus, while each community will generate an architecture that meets its individual needs, the use of IHE profiles will lead to the creation of standards-based communities.
This white paper will focus on explaining how the mCSD Profile can be used to address specific implementation needs. Since mCSD doesn’t require a particular set of FHIR® resources to support, there is a need to define various implementations and the additional requirements they would have. For example, a Facility Registry would require supporting mCSD with Location and Organization resources, and a Health Worker Registry / Provider Directory would require Practitioner resources.
1.2 Intended Audience
The assumed audience for this white paper includes those involved in a current or planned health information community of any size and scope that needs an overview of a framework for building a health information exchange model based on open standards. This white paper does not cover the technical details as they are found in the IHE Profiles, White Papers, and Webinar material.
Some intended audiences include:
- Government (MOH, CDC)
- Federal Health Agencies (ONC, HHS, NIST)
- Regional/State Health Agencies (State Public Health Agencies)
- NGOs (WHO, UNICEF)
- Health Information Exchanges
- Standards Development Organizations
- HIT Non-Profits/Professional Associations (GDHP, HIMSS, RSNA, etc.)
- Health Systems
- Executive Offices (CEO, CIO, CMIO, CNIO, CSO, CTO, CPO, etc.)
1.3 Overview of Mobile Care Services Discovery
The Mobile Care Services Discovery (mCSD) Profile supports discovery of care services resources using a RESTful interface in interrelated, federated environments.
The profile supports querying for:
Organization – Organizations are “umbrella” entities; these may be considered the administrative bodies under whose auspices care services are provided such as Healthcare Information Exchanges (HIEs), Integrated Delivery Networks (IDNs), Non-Government Organizations (NGOs), Faith-Based Organizations (FBOs) or even a one-physician family practice. An organization has a unique identifier and may have additional administrative attributes such as contact person, mailing address, etc. departments of an institution, or other administrative units, may be represented as child Organizations of a parent Organization.
Facility – Facilities are physical care delivery sites such as hospitals, clinics, health outposts, physician offices, labs, pharmacies, etc. A Facility has a unique identifier, geographic attributes (address, geocode), contact attributes, attributes regarding its hours of operation, etc. Each Facility is defined by a pairing of Location and Organization.
Location – Locations are physical places where care can be delivered such as facilities, buildings, wards, rooms, or vehicles. Locations also include jurisdictions such as a village districts or regions. A Location has a unique identifier and may have geographic attributes (address, geocode), attributes regarding its hours of operation, etc. Each Location may be related to one Organization. A location may have a hierarchical relationship with other locations.
Jurisdiction – Jurisdictions are political administrative units or other territories over which authority is exercised. A Jurisdiction has a unique identifier, geographic attributes, etc. Jurisdictions include political administrative units such as village districts or regions. Each Jurisdiction is defined by a pairing of Location and Organization.
Practitioner – A Practitioner is a health worker such as defined by WHO http://www.who.int/whr/2006/06_chap1_en.pdf; a Practitioner might be a physician, nurse, pharmacist, community health worker, district health manager, etc. Practitioners have contact and demographic attributes. Each Practitioner may be related to one or more Organizations, one or more Locations and one or more Healthcare Services. Specific attributes may be associated with the Practitioner relationship with these other entities.
Healthcare Service – Each healthcare service has a unique identifier. Examples include surgical services, antenatal care services, or primary care services. The combination of a Healthcare Service offered at a Location may have specific attributes including contact person, hours of operation, etc.
The relationship between these entities is illustrated in Figure 1.3-1.
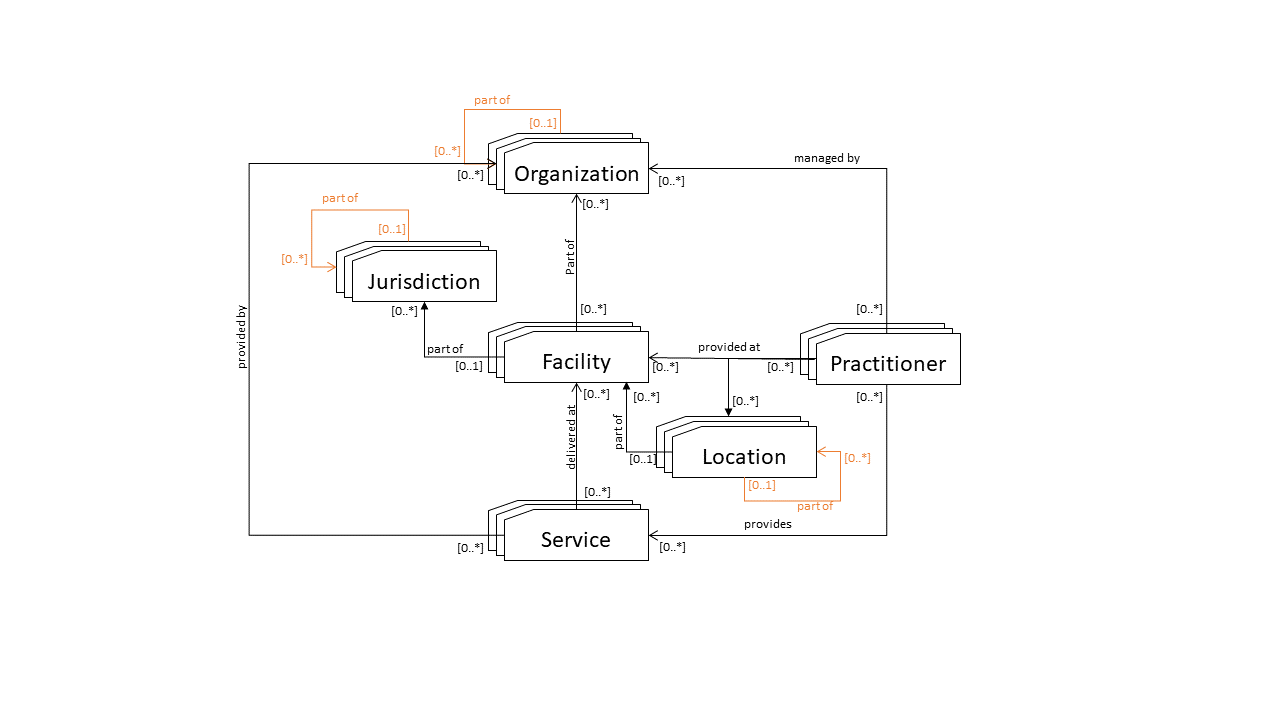
Figure 1.3-1: Top-level Relationships Between Care Service Entities
1.3.1 IHE Terminology
IHE Profiles, including mCSD, use a specific terminology to express use cases: Actors, Transactions, Resources, and Options. This terminology creates a set of interoperability constraints. Actors are the information systems or components of information systems in the workflow. Transactions are the exchanges between Actors. Resources mean FHIR® resources (for FHIR®-centered Profiles). Options in mCSD may exist for Actors which are additional Transactions that may or may not be chosen for the use case.
1.3.2 Use For Authorization
mCSD can be used to assist with authorization by querying for what organizations and/or roles a practitioner is associated with to determine what resources they have access to. When a practitioner needs access, the access control system may use the registry relationships, such as to organizations or roles, to see if they can be given access.
The Access Control White Paper describes these scenarios. mCSD can also be used for attribute retrieval as described in Section 9.5. Section 5.7.2 discusses how PIX/PDQ can be used to retrieve patient attributes for cross-enterprise access control and mCSD can be used to do the same for practitioner attributes.
1.3.3 Facilities and Jurisdictions
First, it is important to say that we often think of health facilities as a single concept, such as physical sites such as hospitals, clinics, health outposts, physician offices, etc. In this way of thinking, a facility has a unique identifier, geographic attributes (address, geocode), contact attributes, attributes regarding its hours of operation, etc.
But, in FHIR® there is no single facility resource, rather, in mCSD, each Facility is defined by a pairing of FHIR Location and FHIR Organization. All of the attributes required can be included, but there is no 'Facility' FHIR resource. mCSD uses the type element in the Location and Organization resources to signify that the resources are being used as a facility or jurisdiction. In the mCSD Supplement, see Tables 3.90.4.2.2.1-2 and 3.90.4.2.2.2-2 for Facilities and Tables 3.90.4.2.2.1-3 and 3.90.4.2.2.2-3 for Jurisdictions.
A facility is defined as a FHIR Location + FHIR Organization pair
The key takeaway is that when thinking of a health facility, there is no single FHIR resource, instead it is represented in FHIR® as a Location and Organization resource pair linked by the
Location.managingOrganizationelement. Jurisdictions are handled the same way.
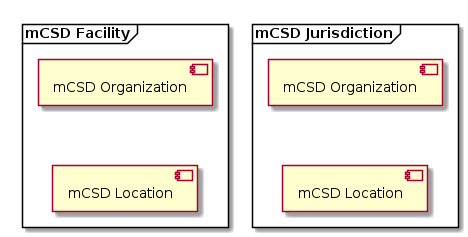
Figure 1.3.3-1: Facilities and Jurisdictions
- FHIR Locations are physical places where care can be delivered such as facilities, buildings, wards, rooms, or vehicles. Locations also include political administrative units such as a village districts or regions. A Location has a unique identifier and may have geographic attributes (address, geocode), attributes etc. Each Location may be related to one Organization. A location may have a hierarchical relationship with other locations.
Locations only relate to one organization
The key takeaway is that a FHIR Location doesn't have enough details to describe the management side of the facility and that's where Organization comes in.
- FHIR Organizations are "umbrella" entities; these may be considered the administrative bodies under whose auspices care services are provided such as Healthcare Information Exchanges (HIEs), Integrated Delivery Networks (IDNs), Non-Government Organizations (NGOs), Faith-Based Organizations (FBOs) or even a one-physician family practice. An organization has a unique identifier and may have additional administrative attributes such as contact person, mailing address, etc. Departments of an institution, or other administrative units, may be represented as child Organizations of a parent Organization.
Organizations can have more than hierarchy, but not Locations
Organizations are powerful representations, they can have more than one hierarchy in mCSD, but Locations can only have one hierarchy. (This requires an mCSD extension to the core FHIR® spec for Organizations.)
1.3.3.1 Hierarchies
Multiple hierarchies are handled with a FHIR® extension on the Organization resource in mCSD. Each Organization can be part of any number of parent Organizations associated with a type for the hierarchy. A hierarchy can be within Facilities, Jurisdictions and/or Organizations. This extension is described in Table 3.90.4.2.2.1-1 of the mCSD Supplement.
Clients to the facility registry can search based on the hierarchy type and parent Organizations.
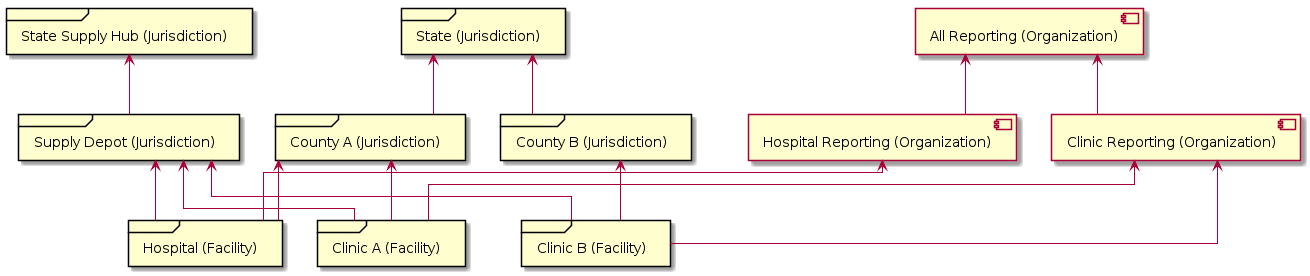
Figure 1.3.3.1-1: Multiple Hierarchies
2 Key Use Cases
The existing use cases all give good examples of specific implementations, such as:
2.1 Master Facility List
A developing country has decided to implement a Master Facility List (MFL) based on recommendations from the WHO in the MFL Resource Package. This resource includes a minimum data set to uniquely identify, locate, and contact a specific facility. Since this will be a single source of information for the country, there may be differing hierarchies that need to be supported for the facilities. For example, one hierarchy would be the administrative hierarchy for the country (region, district, county). Another would be the supply chain hierarchy where hubs may be located separately from administrative regions. Yet another could be a reporting hierarchy used to send data to health system managers, and on up to international organizations.
2.1.1 Implementation
Solution Option: Simple Facility Registry
The MFL can implement a Simple Facility Registry as a sole source of the facility data. Clients can then query that data. The MFL can utilize mCSD Facilities and Jurisdictions with multiple hierarchies.
2.2 Care Services Registry
To support health system planning, resource management, and patient referral workflows, it will be important to be able to relate healthcare facilities with the health services that are provided there by practitioners. A care services registry may be operationalized that leverages mCSD to cross-reference a code list of health services with the unique list of facility IDs. Such a cross reference may include information related to service provision availability (days and times of day).
2.2.1 Implementation
Solution Option: Care Services Registry
This Care Services Registry supports all the information contained in mCSD in a federated environment. Data can be managed in separate registries and combined in the care services registry for managed access to the complete data set. A Health Worker Registry and/or a Federated Facility Registry can send data updates to the care services registry. There can be multiple data sources, for example from private and public hospitals. Internal business processes can be used by the care services registry to link this data or reconcile duplicates as needed. Clients can then query the combined data set without requiring access to the various data sources.
2.3 Health Worker Registry
A Health Worker Registry could be operationalized by collecting and collating underlying provider demographic content from multiple clinical colleges (e.g., College of Physicians and Surgeons, College of Nurses, College of Pharmacists, etc.). These Colleges exert governance over their membership, which may include a requirement of licensure in the self-governing body in order to legally practice in a jurisdiction. As such, the underlying Colleges will maintain the content and a Health Worker Registry would periodically refresh its content from these multiple underlying sources and execute necessary cross-referencing and de-duplication workflows to support an care services registry relating WHICH workers (Practitioner) provide WHAT SERVICES (HealthcareService), WHERE (Location).
Unlicensed Practitioner Roles and the Community and Volunteer Health Workforce
In FHIR®, a Practitioner is a "person who is directly or indirectly involved in the provisioning of healthcare". This means that some Practitioners may be in roles that require qualifications and licensure to perform in a jurisdiction, while other Practitioners providing care may not, and still others may engage in support functions. One example may be a nurse's aide who may not require licensure or formal qualification but are providing care. Another example is that in Low- and Middle-Income Countries (LMIC) the formal health workforce is often supplemented by volunteers as in vaccination campaigns and Community-based Health Workers (CHWs) to support maternal and child health. Some examples of support functions from the FHIR® R4 Practitioner specification are receptionists and IT personnel.
The mCSD Profile adopts the FHIR Practitioner approach in that all direct and indirect roles in healthcare may be captured in Practitioner and PractitionerRoles. Implementers of mCSD may choose to pursue their own formal definitions of the health workforce and define them, for example in ValueSets, in their Implementation Guides.
2.3.1 Implementation
Solution Option: Federated Health Worker Registry
A central federated health worker registry can be set up that pulls data from various other sources of practitioner data such as the clinical colleges and licensing boards. Data can also be pulled from HR systems and combine this data with the licensing and training data.
2.4 Functioning Facilities Registry
Monitor functioning facilities, e.g., when buildings are operational, construction teams, infrastructure, maintenance, then share that information with the public. There is a need to immediately view services, openings, closures.
2.4.1 Implementation
Solution Option: Simple Facility Registry
This registry is an extension of the Master Facility List to include services data for the facilities. It would also include the times those services are available so it can be used to look up locations for referrals. It can also be used internally to track work and closures of the facilities.
2.5 Federated Facility Registry
A common problem is that multiple data systems are collecting information about facilities. For example, in one country, there are 6 DHIS2 platforms that are not aligned, and are struggling to maintain metadata.
2.5.1 Implementation
Solution Option: Federated Facility Registry
There can be a central federated facility registry that can pull data from the DHIS2 platforms and integrate it. Once the data has been aligned, it can then be used to update the source systems based on internal policies.
2.6 Federated Data Collection
A way is needed to integrate some regular, large data collections (HHFA) from surveys which visit all facilities in the country, and these data sources are not connected to the maintenance of the facilities. One should be able to integrate information from large data collection.
2.6.1 Implementation
Solution Option: Federated Facility Registry
The data collection systems can support mCSD to share the collected data to the central facility registry.
2.7 Aggregate Data Reporting
Aggregate data reporting refers to routine reporting, often from a health facility, to an administrative jurisdiction, health financing entity, or external donors and investors.
As an example use case, a donor invests in vertical public health programs for epidemic control across many countries. The donor has a multi-country dashboard and analytics platform that aggregates data and tracks progress of program outcomes at the facility level There are within-country facility IDs issued by the Ministry of Health, and IDs for facilities used by the multi-country analytics platform. IDs may change, temporary facilities like immunization sites may be added, administrative hierarchies may split, and facilities may drop or be upgraded to another level of clinical care over time. A similar use case could arise in a country in which public healthcare is decentralized and provided and overseen by subnational political units who engage in routine reporting to the national authority.
Solution Option: Federated Facility Registry
3 Facility Registry
A Facility Registry can provide data on facilities in a particular area. Optionally, it can provide details on what healthcare services are supplied by those facilities. Sometimes this data may be managed by multiple services and the content can be federated so information can be accessed from a central system, but managed locally.
3.2 Implementations
3.2.1 Simple Facility Registry
A Simple Facility Registry will allow any searches on its facility data. It manages it's own data and doesn't receive data updates from other services. It will contain Location and Organization data to reference mCSD Facilities and Jurisdictions as well as any other non-jurisdictional Organizations. It will also include geographic data so searches can also be done by distance. It will optionally include healthcare service content.
The following actors, transactions, and resources are be used.
- Actors (Options)
- Care Services Selective Supplier (Location Distance Option)
- Transactions
- Find Matching Care Services [ITI-90]
- Resources
OrganizationLocationHealthcareServiceOptional
Clients will act as a Care Services Selective Consumer (Location Distance Option) to search the Facility Registry content. Figure 3.2.1-1 shows a Health Management Information System (HMIS) and a Mobile App querying the Facility Registry using Find Matching Care Services [ITI-90].
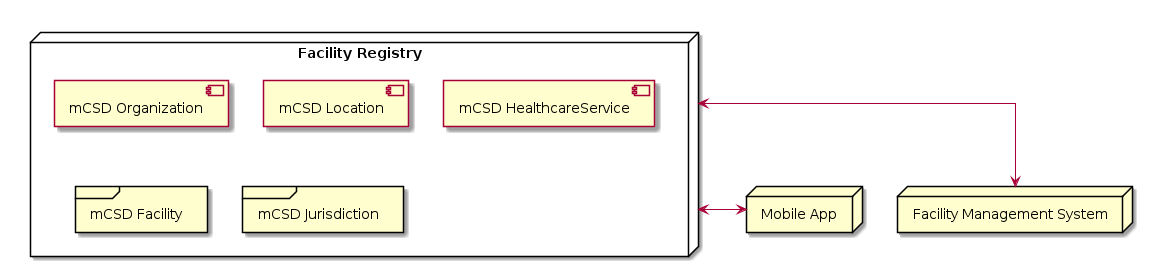
Figure 3.2.1-1: Simple Facility Registry
Figure 3.2.1-2 shows the sequence of requests to and from the HMIS and Mobile App to the Facility Registry.
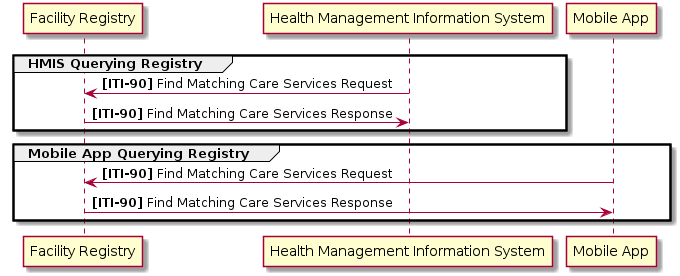
Figure 3.2.1-2: Simple Facility Registry Transaction Sequence
3.2.2 Federated Facility Registry
In a distributed environment, some aspects of the facilities are managed in multiple systems so they need to be federated using Request Care Services Updates [ITI-91]. Some systems may also need to pull full updates from the registry instead of searching. A federated facility registry can optionally include healthcare service content.
The following actors, transactions, and resources are be used.
- Actors (Options)
- Care Services Selective Supplier (Location Distance Option)
- Care Services Update Supplier (Location Distance Option)
- Care Services Update Consumer (Location Distance Option)
- Transactions
- Find Matching Care Services [ITI-90]
- Request Care Services Updates [ITI-91]
- Resources
OrganizationLocationHealthcareServiceOptional
Other sources will act as a Care Services Selective Suppliers (Location Distance Option) to update the Facility Registry content. Figure 3.2.3-1 shows a federated system of servers sending their content to a Federated Facility Registry using Request Care Services Updates [ITI-91] and a mobile app querying facility data using Find Matching Care Services [ITI-90]. Each server can also pull the full combined data set from the Facility Registry as a Care Services Update Consumer as needed.
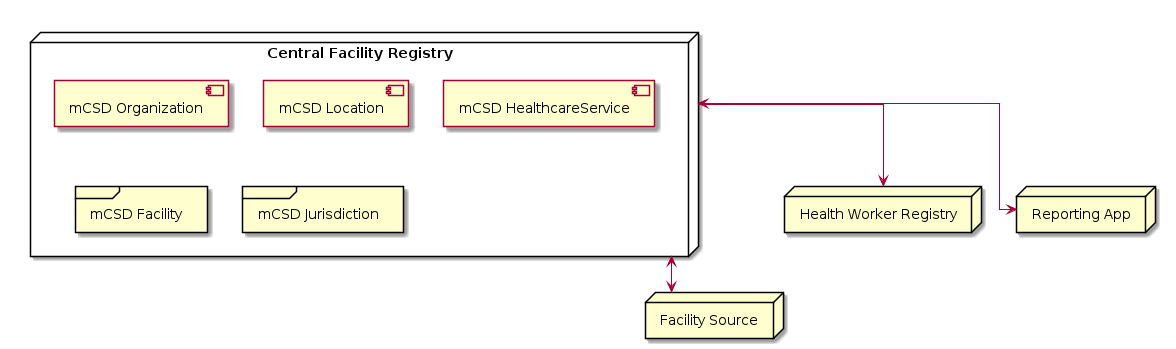
Figure 3.2.2-1: Federated Facility Registry
Figure 3.2.2-2 shows the sequence of requests to and from the Registry and the various sources as well as a mobile app querying the entire data set.
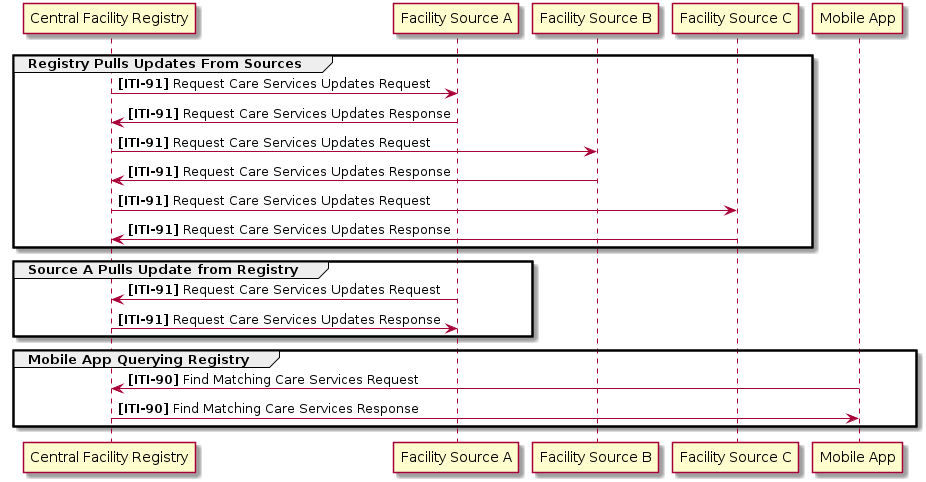
Figure 3.2.2-2: Federated Facility Registry Transaction Sequence
4 Health Worker Registry
4.1 Implementations
4.1.1 Simple Health Worker Registry
A Simple Health Worker Registry will allow any searches on its health worker data. It will contain Practitioner and PractitionerRole data and optionally HealthcareService data.
The following actors, transactions, and resources are be used.
- Actors (Options)
- Care Services Selective Supplier
- Transactions
- Find Matching Care Services [ITI-90]
- Resources
PractitionerPractitionerRoleHealthcareServiceOptional
Clients will act as a Care Services Selective Consumer to search the Health Worker Registry content. Figure 4.1.1-1 shows a Health Management Information System (HMIS) and a Mobile App querying the Health Worker Registry using Find Matching Care Services [ITI-90].
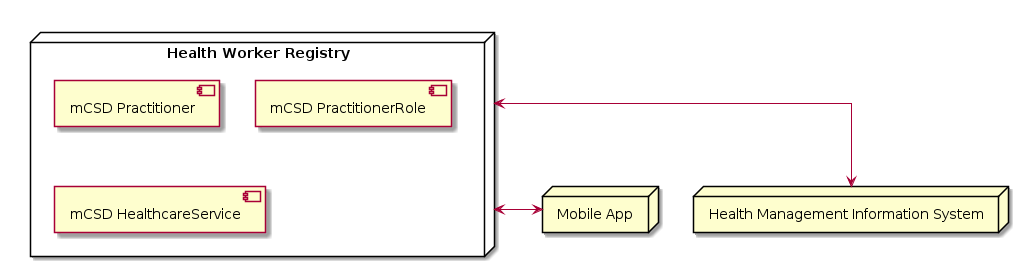
Figure 4.1.1-1: Simple Health Worker Registry
Figure 4.1.1-2 shows the sequence of requests to and from the HMIS and Mobile App to the Health Worker Registry.
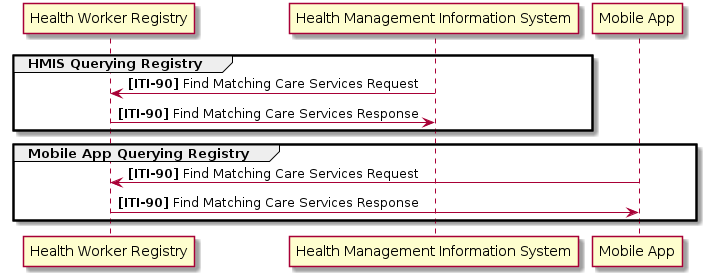
Figure 4.1.1-2: Simple Health Worker Registry Transaction Sequence
4.1.2 Federated Health Worker Registry
In a distributed environment, some aspects of the health workers are managed in multiple systems so they need to be federated using Request Care Services Updates [ITI-91]. Some systems may also need to pull full updates from the registry instead of searching. It will optionally include healthcare service content.
The following actors, transactions, and resources are be used.
- Actors (Options)
- Care Services Selective Supplier
- Care Services Update Supplier
- Care Services Update Consumer
- Transactions
- Find Matching Care Services [ITI-90]
- Request Care Services Updates [ITI-91]
- Resources
PractitionerPractitionerRoleHealthcareServiceOptional
Other sources will act as a Care Services Selective Suppliers to update the Health Worker Registry content. Figure 4.1.3-1 shows a federated system of servers sending their content to a Federated Health Worker Registry using Request Care Services Updates [ITI-91] and a mobile app querying health worker data using Find Matching Care Services [ITI-90]. Each server can also pull the full combined data set from the Health Worker Registry as a Care Services Update Consumer as needed.
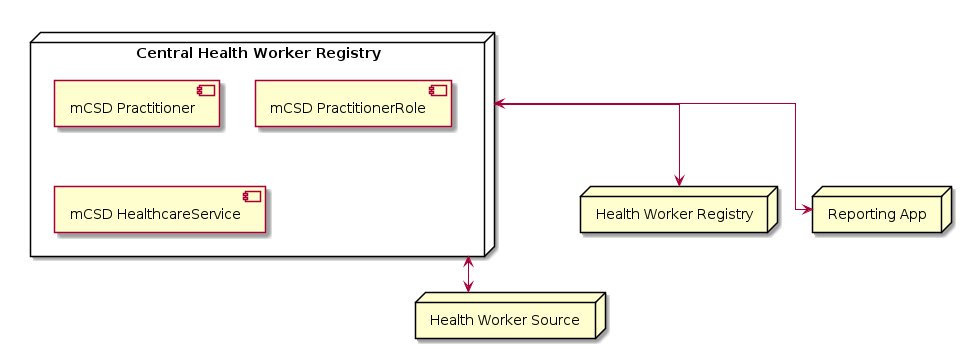
Figure 4.1.2-1: Federated Health Worker Registry
Figure 4.1.2-2 shows the sequence of requests to and from the Registry and the various sources as well as a mobile app querying the entire data set.
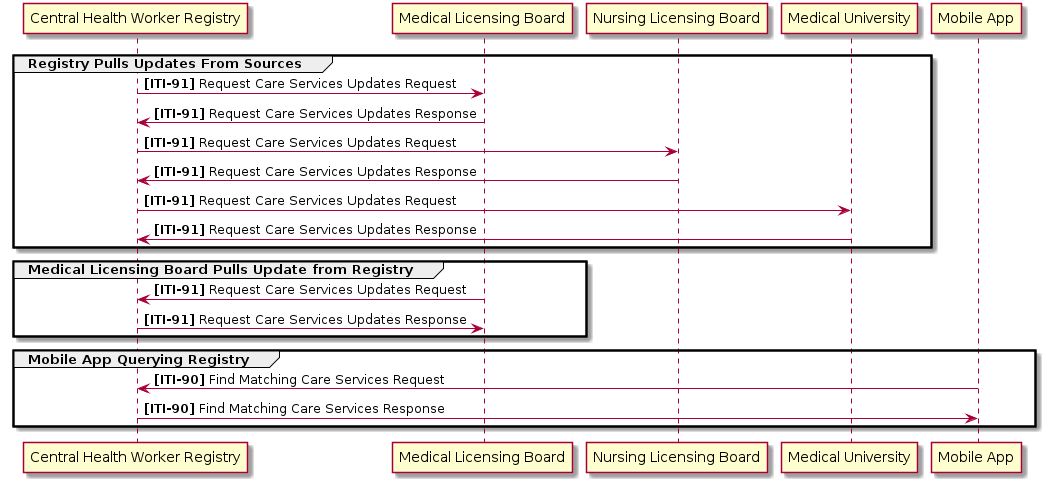
Figure 4.1.2-2: Federated Health Worker Registry Transaction Sequence
5 Care Services Registry
Care Services Registries include data on facilities as well as practitioners and can optionally include healthcare services.
5.1 Facilities and Jurisdictions
See the Facility Registry for Facilities and Jurisdictions
5.2 Implementations
5.2.1 Care Services Registry
In some instances, all the care services data would be combined into a single central server for easier access. In most cases this server would pull data from various source servers (such as a Facility Registry or Health Worker Registry) and link the resources together. This registry may also include healthcare service content.
The following actors, transactions, and resources are be used.
- Actors (Options)
- Care Services Selective Supplier (Location Distance Option)
- Care Services Update Supplier (Location Distance Option)
- Care Services Update Consumer (Location Distance Option)
- Transactions
- Find Matching Care Services [ITI-90]
- Request Care Services Updates [ITI-91]
- Resources
OrganizationLocationPractitionerPractitionerRoleHealthcareServiceOptional
Other sources will act as a Care Services Selective Suppliers to update the Care Services Registry content. Figure 5.2.1-1 shows a federated system of servers sending their content to a Federated Care Services Registry using Request Care Services Updates [ITI-91] and a mobile app querying data using Find Matching Care Services [ITI-90]. Each server can also pull the full combined data set from the Care Services Registry as a Care Services Update Consumer as needed.
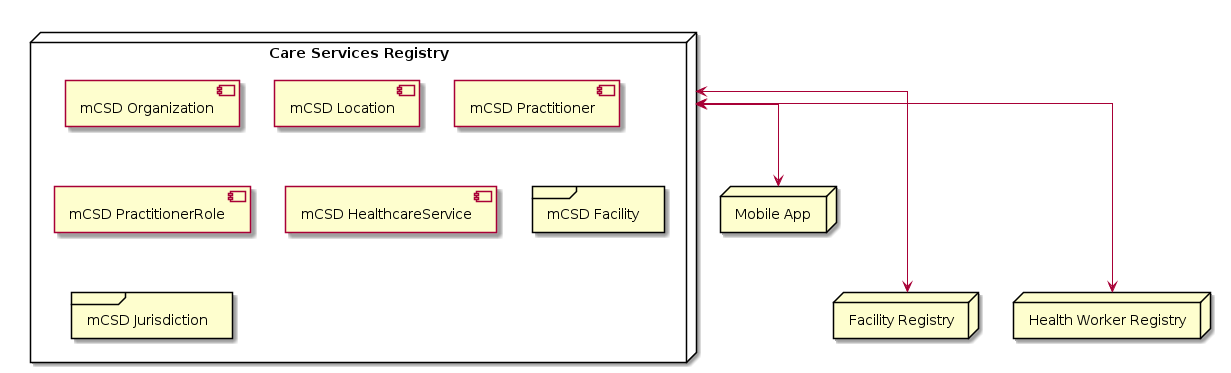
Figure 5.2.1-1: Federated Care Services Registry
Figure 5.2.1-2 shows the sequence of requests to and from the Registry and the various sources as well as a mobile app querying the entire data set.
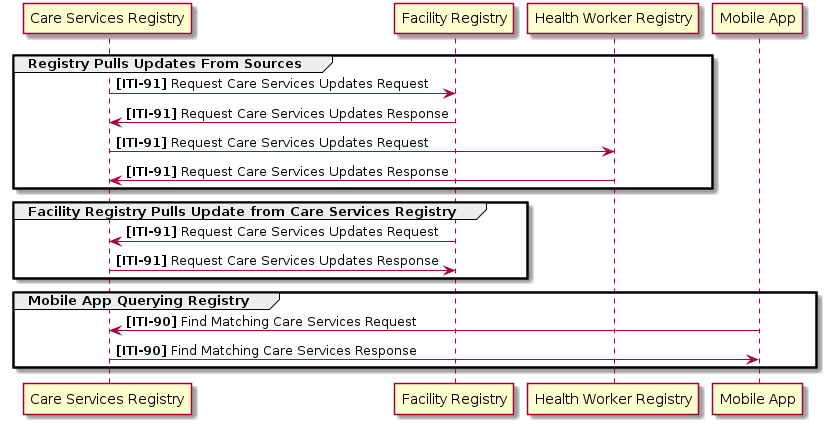
Figure 5.2.1-2: Federated Care Services Registry Transaction Sequence
